Types of Pancreatic Cancer
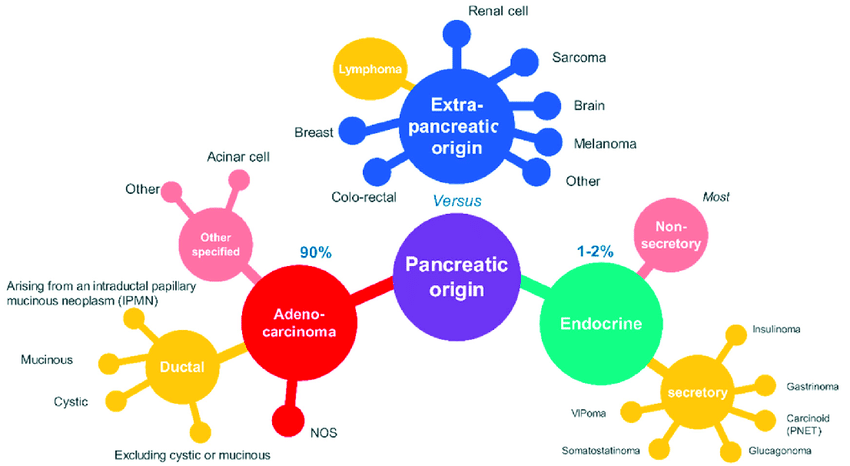
A mass was palpated in the head of the pancreas. A biopsy confirmed that it was a tumor. Its presence required surgery. In most cases, surgery is not needed. If cancer is present, it may not be dangerous. But it is crucial to know the signs and symptoms of the various types of pancreatic tumors to choose the proper treatment for your condition. In this article, you'll learn about the most common types of pancreatic cancer.
Mesothelial cysts
Pancreatic pseudocysts are the most common type of non-neoplastic pancreatic cyst. They are circumscribed sacs of fluid containing pancreatic enzymes. Pseudocysts are often associated with pancreatitis, a condition where the digestive enzymes in the pancreas become too active to function correctly. In addition, pseudocysts are caused by separating the ventral pancreatic duct and its side branches. This condition is also known as pancreatic parenchymal necrosis.
There are now many diagnostic methods for pancreatic cysts, including magnetic resonance imaging, multidetector computed tomography, and cholangiopancreatography. While these advanced diagnostic methods have increased the ability to detect pancreatic tumors, they may also increase healthcare costs. In addition, incidental detection of pancreatic cysts is often a frightening experience for patients and a source of anxiety for gastroenterologists. Unfortunately, pancreatic cysts can be benign or borderline malignant.
Serous cystadenomas
A 73-year-old female presents with a lobulated, honeycomb-like serous cystadenoma in the head of the pancreas. Axial IV contrast-enhanced CT shows several small cysts separated by thin fibrous septa. The gross pathology photograph shows a honeycomb-like pattern of microcysts with a central fibrous scar. The presence of cysts in the head of the pancreas is characteristic of serous cystadenomas.
The diagnosis of serous cystadenomas is based on a variety of clinical characteristics and can be derived from a patient's family history and physical exam. Most patients are considered benign and diagnosed incidentally during a cross-sectional imaging procedure. However, doctors should ask the patient about their family history to rule out hereditary syndromes or other diseases associated with pancreatic lesions. Moreover, patients should be counseled about any new symptoms that occurred in the past because these may indicate a more complex illness or a pancreatic tumor.
Endocrine tumors
Neuroendocrine tumors of the pancreas (PNET) are relatively rare endocrine tumors. They begin in the endocrine cells of the pancreas and tend to increase. Pancreatic NETs are usually sluggish, but they can be malignant. The biological behavior of individual PNETs is variable, and diagnosis is essential. The aggressive treatment of pancreatic NETs requires imaging and endocrine tests.
Neuroendocrine tumors begin in the endocrine cells of the pancreas, which make hormones that regulate blood sugar and digestion. The pancreas also has exocrine cells, which produce enzymes that break down food. The pancreas has many types of neuroendocrine tumors. The most common type is insulinoma, which causes the pancreas to make too much insulin. This can cause symptoms such as fatigue, blurred vision, and rapid heartbeat.
Papillary mucinous neoplasms
Papillary mucinous nidi of the head of the pancreas is a spectrum of neoplasms involving the head of the duct of the pancreas. They are classified as either benign or malignant and are usually associated with dilated pancreatic ducts. Patients with this type of tumor have a 50% chance of developing pancreatic cancer. This type of tumor is not usually associated with symptoms but is often diagnosed during tests for other conditions.
Surgical resection is the treatment of choice for most IPMNs. The preoperative determination of the presence of associated invasive cancer is critical. Regional lymph node resection may also be necessary. The spectrum of appearances of papillary mucinous neoplasms of the head of the pancreas is described in a retrospective review of 64 patients.