Symptoms of Autoimmune Thyroiditis
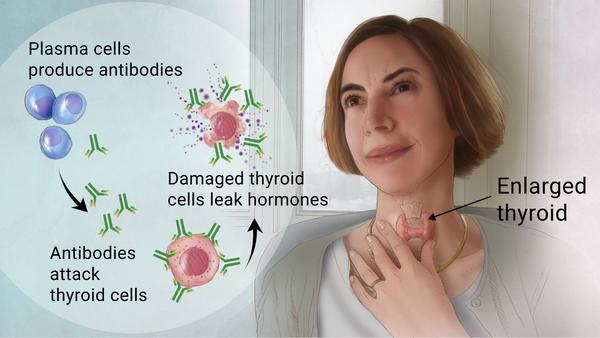
A person with autoimmune thyroiditis (AT) is more likely to develop another autoimmune disease. However, the vast majority of patients will only develop thyroiditis. There are many symptoms associated with AT. Some people experience a swollen, enlarged thyroid gland. Other people may experience a decrease in their thyroid's ability to produce thyroid hormones. In many cases, the thyroid may not have enough hormones to meet the body's demands.
Hashimoto's thyroiditis
Hashimoto's thyroiditis is an autoimmune disease that causes an enlargement of the thyroid gland. The swelling causes the throat to feel full and can interfere with swallowing and breathing. It can also be painful. If left untreated, Hashimoto's thyroiditis can lead to the development of myxedema, a rare type of hypothyroidism. People with this condition are also more likely to develop other autoimmune disorders, including type 1 diabetes and rheumatoid arthritis. Symptoms of Hashimoto's thyroiditis may include a bulge in the neck, throat pain, difficulty swallowing, breathing, and speaking.
Hashimoto's thyroiditis can be diagnosed through laboratory tests. Your doctor will check your thyroid hormone levels and determine if treatment is necessary. If you have a low TSH level, you'll need to take a thyroid hormone supplement, such as Levothyroxine. The medication is usually taken for life, so monitoring your thyroid hormone levels regularly is important.
Graves' disease
The causes of Graves' disease are not fully understood, but several clinical features and imaging techniques can help diagnose this condition. Several treatment options are available for people suffering from Graves' disease. Large volumes of clinical data support the decision-making process.
Graves' disease is an autoimmune disease. It is caused by circulating antibodies that mimic the thyroid-stimulating hormone (TSHR) effects. Although the exact cause is still unknown, genetics and environmental factors play a role.
Lymphocytic thyroiditis
Lymphocytic thyroiditis is a thyroid gland disorder that often occurs in postpartum women. It can affect as many as 6% of women within 2-12 months after delivery. The condition's onset is often unprovoked, and the thyroid hormone levels return to normal after a short period. It is also associated with increased circulating anti-thyroid antibodies and type 1 diabetes. The resulting symptoms are typically characterized by transient hypothyroidism lasting two to eight weeks. The autoimmune component is thought to be the culprit.
Lymphocytic thyroiditis is an autoimmune disorder that affects the production of thyroid hormones. This condition is usually asymptomatic, and the symptoms are often overlooked until an examination is performed. Reduced thyroid function includes nervousness, easy fatigue, drowsiness, and insomnia. Sometimes the affected thyroid gland becomes enlarged and becomes nodular.
Drug-induced thyroiditis
Drug-induced thyroiditis is often a side effect of a certain medication. Patients may experience pain around the thyroid that can be managed with ibuprofen or other drugs. However, in severe cases, steroids may be necessary. Radiation or chemotherapy treatment to the thyroid gland may also damage the thyroid gland. This can lead to either over or under-production of thyroid hormones. In either case, the condition can be permanent and require long-term treatment. On the other hand, infectious thyroiditis is usually caused by a bacterial infection. Children with this condition typically have a weakened immune system and a problem with developing the thyroid gland.
In addition to this, autoimmune thyroiditis may cause the thyroid to fail to function correctly. Therefore, patients who have this condition should be tested for the presence of thyroid antibodies. Thyroid ultrasounds are also useful to detect abnormalities in the thyroid. If either of these conditions is present, a follow-up evaluation will be necessary to treat the situation appropriately.