Pancreatic Neoplasia
Pancreatic neoplasia (Pancreatic cancer) is a rare condition in which pancreatic cells become abnormal. Its symptoms, diagnosis, and treatment are described in this article. If you suspect you may have Pancreatic cancer, speak with your doctor or family doctor. Screening for Pancreatic cancer is crucial to detect it early. To avoid the condition's complications, check your doctor regularly.
Symptoms
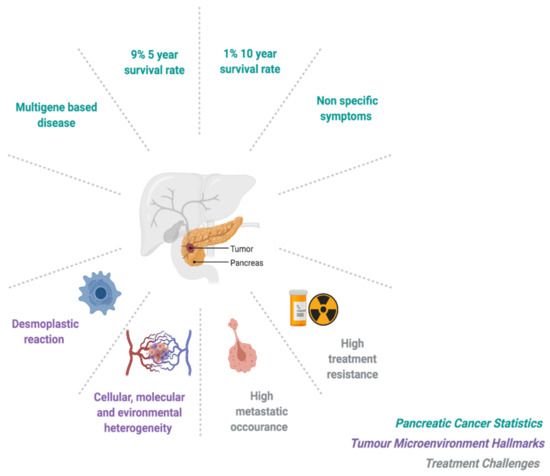
The main symptoms of pancreatic cancer include abdominal pain and yellowing of the skin. The initial symptoms of pancreatic neoplasms are usually nonspecific and easily mistaken for other diseases or processes. Therefore, a physician must have a high index of suspicion when looking for these symptoms. However, the doctor should immediately perform a CT scan or ultrasound to confirm the diagnosis if these symptoms are present. Once the diagnosis is confirmed, treatment will begin.
The most common type of pancreatic cancer is adenocarcinoma, which affects approximately 32,000 people yearly. The survival rate for the locally resected disease is 17 per cent. Smoking and specific cancer syndromes, such as chronic familial pancreatitis, are associated with an increased risk of developing this type of cancer. Patients typically present with epigastric pain and weight loss, but more than half will also have distant metastasis.
Diagnosis
Despite the difficulty of detecting premalignant lesions in a small patient sample, imaging tests have the potential to diagnose the disease and detect metastases to other organs. However, these tests are not sensitive enough to detect lesions just a few millimetres in diameter. Because of this, premalignant lesions must be histologically confirmed.
In one study, 737 patients were referred to a pancreatic surgeon for evaluation of a mass in the pancreas. Five hundred and sixty FNA-sampled lesions were identified, of which 480 were adenocarcinomas, and two were serous cystadenomas. The sensitivity of EUS-FNA to diagnose pancreatic cancer was 77%, whereas its sensitivity was 68% for detecting suspected malignancy.
Treatment
Although pancreatic cancer cannot be cured, palliative treatments are available to minimize the pain and symptoms of the disease. Pancreatic neoplasia patients may undergo chemotherapy, radiotherapy, or drug therapies. Treatments for advanced pancreatic cancer may involve chemotherapy, radiation therapy, supportive care, and psychosocial support. Patients may be seen by their GP, who will monitor their general health and coordinate treatment. Other specialists, including medical or radiation oncologists, will coordinate and prescribe medicines. Other allied health professionals, including social workers or pharmacists, will help patients cope with their disease.
Patients with early-stage disease are treated with radiation therapy and chemotherapy. In stage III tumours, chemotherapy is usually used. Surgery to remove the pancreas may be combined with radiation therapy. Patients with advanced cancer are treated with targeted therapies. Surgery is not often performed for stage II pancreatic neoplasia but may be performed in patients with progressive disease. It is important to note that radiation therapy is only used if the tumour is resistant to radiation.
Screening
While population-wide screening for pancreatic cancer has some benefits, the cost-effectiveness of such a scheme is in doubt. Current testing modalities have low positive predictive values and generate a high rate of false positives, resulting in an unacceptable number of false negatives. Consequently, many experts advocate screening only for individuals at increased risk of developing pancreatic cancer. But which screening modalities are most accurate?
Generally, screening is best performed if an individual is a member of an FPC family or has a family history of pancreatic cancer. Those with germline genetic mutations are also at an increased risk. Genetic counselling is an excellent choice to help patients understand their risks and decide whether further testing is needed. Screening may be recommended for people diagnosed with a benign intraductal papillary mucinous neoplasm (IPMN). If the imaging indicates growth, doctors may recommend treatment and ongoing screening.