Pancreatic Ductal Adenocarcinoma
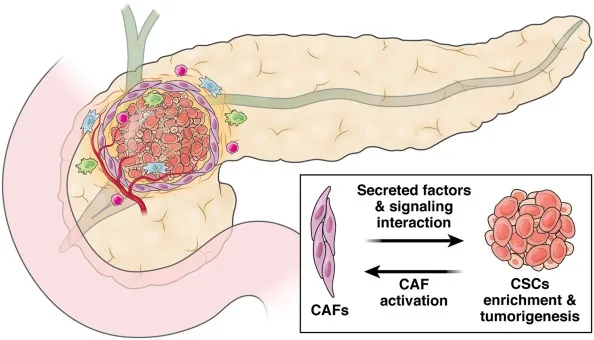
Although pancreatic ductal adenocarcinoma (PDA) is one of the most aggressive solid tumours, it is not genetically homogeneous. While Molecular PDA subtypes have been proposed but are not yet driving clinical treatment decision-making, we know that the tumour microenvironment plays a significant role in the progression and response to chemotherapy. We know that the tumour stroma may also play a role in progression. Identifying these features and their prognostic significance may be essential for advancing precision oncology.
Pathology
Pancreatic ductal adenocarcinoma (PDAC) is a highly aggressive form of cancer that typically has a poor prognosis. Although it is often curable with surgery, only a minority of patients achieve a cure. This article examines the pathology, cytology, and molecular testing used to diagnose PDAC. We also highlight the importance of consulting a specialized centre if you suspect you have the disease.
Pancreatic ductal adenocarcinomas have a poor prognosis, and recent data suggest that molecular subtypes may differ in their clinical outcomes. One recent study looked at the association between histopathologic heterogeneity and survival time. One hundred seventy-seven resected PDAC tumours were analyzed and subclassified by the predominant growth pattern. The study found that 95% of patients with PDAC had genetic alterations in two of four genes. Patients with dominant cribriform components had more prolonged survival significantly compared to conventional and combined PDACs.
Diagnosis
The prognosis for patients with pancreatic ductal adenoids is poor. As a result, surgical resection is the mainstay of treatment. Unfortunately, most patients with PDAC present with an advanced stage of the disease. Early-stage PDAC tumours are usually asymptomatic and not detected on abdominal CT examinations.
Diagnosis of pancreatic adenocarcinoma is difficult despite advances in clinical evaluation. The poor collection of tissue makes the pathological diagnosis difficult. ICCs and IDCs, adenocarcinomas that develop in the desmoplastic stroma, are often present in pathological specimens. Although adenoma and cancer are the same, the presence of atypical cells may make the diagnosis difficult.
Treatment
There are currently no approved treatments for pancreatic ductal adenocarcinoma (PDAC), one of the pancreas's most common and aggressive malignancies. The disease's poor prognosis is partly due to its inherited heterogeneity and dense stromal environment. At presentation, only complete surgical resection can cure the disease, and treatment options are limited. In recent years, research into immunotherapy for pancreatic cancer has shown promising results. However, more research is needed.
A recently developed small molecule named selinexor has demonstrated potent antiproliferative activity in the pancreatic cancer cell line MiaPaca-2. It works by disrupting mTOR, a critical signalling pathway in pancreatic ductal adenocarcinoma. Combined with standard treatments, this drug has shown double and triple-digit survival in metastatic PDAC patients.
Survival
Despite the advances in cancer therapy, pancreatic ductal adenocarcinoma (PDAC) is still one of the deadliest cancers. The survival of patients with PDAC has remained essentially the same for decades. The effective primary treatment is surgical resection and subsequent radiation. Chemotherapy is also effective in about 80% of patients.
Researchers have recently compiled and reviewed data on pancreatic ductal adenocarcinoma survival. The Kaplan-Meier survival curve shows the prognosis of patients with and without localized cancer. The survival rate of patients with distant metastases is also shown. These studies demonstrate that treatment is a significant factor in patients' survival.




