Pancreatic Cancer Screening
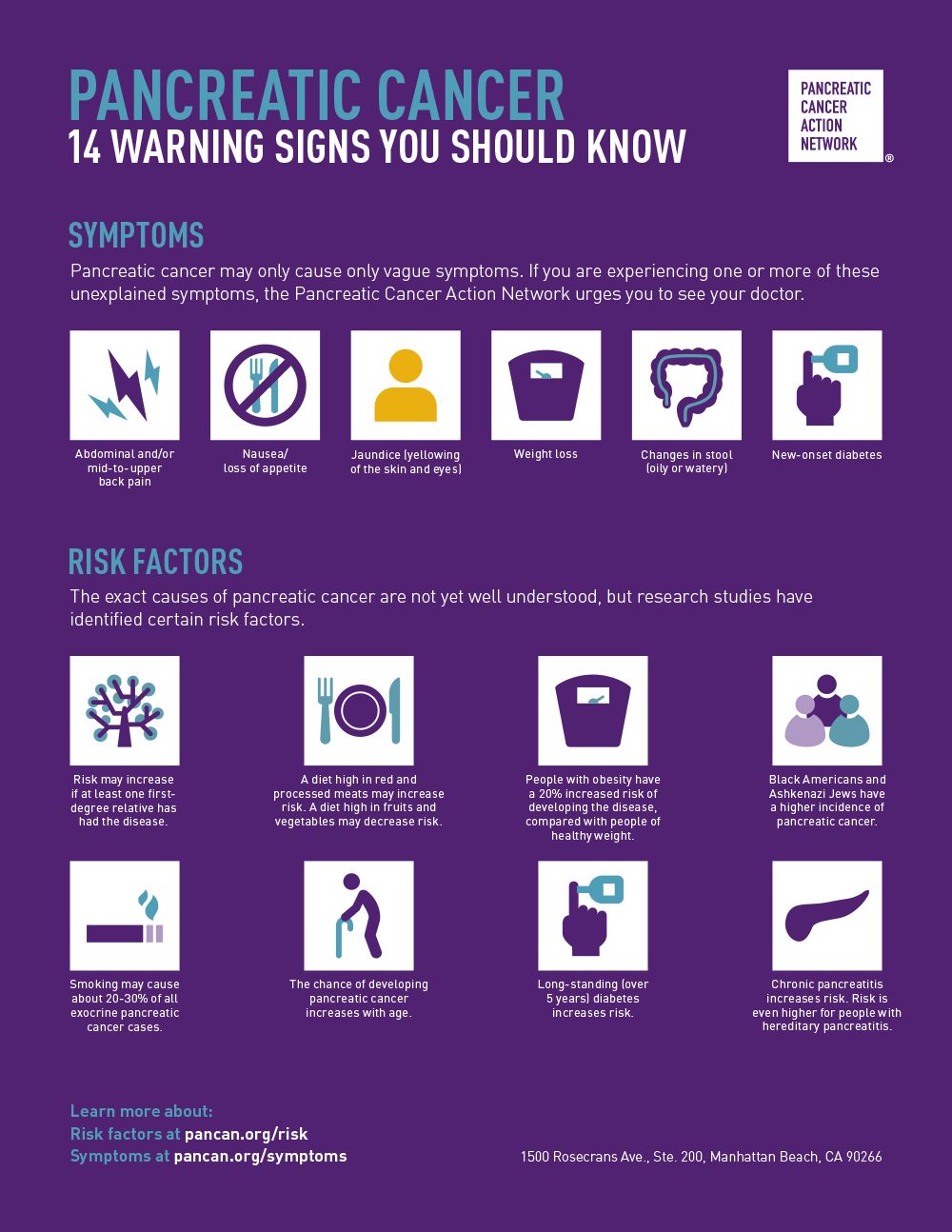
Those who are at high risk for pancreatic cancer include those with certain familial or inherited genetic syndromes. They also have persons with new-onset diabetes, obesity, and a history of chronic pancreatitis but do not necessarily meet the criteria for high risk. Although the USPSTF recommendations do not represent official U.S. government policy, they indicate that specific tests or procedures may have a role in detecting pancreatic cancer.
Endoscopic ultrasound
A physician may use endoscopic ultrasound to detect pancreatic tumours. The process helps visualize the tumour and surrounding blood vessels and structures. It also allows a needle to be passed into the suspected tumour. The hand is then used to collect tissue samples to determine whether the cells are cancerous. The results of this procedure may alter the treatment sequence. For this reason, it is an essential tool in diagnosing and managing pancreatic cancer.
Pancreatic cancer is a severe disease, but early detection of small tumours may significantly reduce mortality. The most sensitive imaging modality for pancreatic lesions, endoscopic ultrasound (EUS), is available today. Because of its high resolution, EUS can identify small pancreatic tumours that other imaging modalities might miss. Because of its accuracy, EUS should be used for screening high-risk individuals.
Magnetic resonance imaging
A screening protocol based on MRI is an excellent way to detect pancreatic cancer, especially premalignant lesions, with high accuracy. Its use as a screening tool reduces costs and increases accessibility while guaranteeing patient safety. In addition, an MRI-based screening protocol provides more information for further synthetic analysis. However, it remains to be seen whether this screening protocol is effective for the general population.
MRI images of the pancreas look similar to those of a CT scan. MRI takes several organ pictures and combines them into a three-dimensional scan. MRI takes longer than CT scans because patients are positioned motionless in a cylinder. It also provides a similar concept to an ERCP without requiring an invasive procedure. MRI and EUS are used to diagnose IPMN.
Blood test
A blood test for pancreatic cancer can detect the most common type of pancreatic cancer in its early stages. This test can help doctors stage the disease and guide treatment choices. A recent multidisciplinary study at the University of Pennsylvania found that liquid biopsy was more accurate than imaging alone. To learn more, read on. Here are some benefits of this test. Listed below are some pros and cons.
If you suspect that you have pancreatic cancer, get tested right away! The first test used to diagnose pancreatic cancer is a blood test called a Cx-45. It checks the protein level called CA 19-9 in the pancreas. Other tests may include CEA or a blood test called CA 19-9. These tests are available without insurance or a doctor's note.
Endoscopic retrograde cholangiopancreatography
Pancreatic cancer may be detected by an endoscopic procedure called endoscopic retrograde cholangiopancreatography. The endoscope is inserted through the mouth and is passed down the oesophagus, duodenum, and stomach. The patient swallows the endoscope as it passes through. A small amount of dye or air may be given to aid in the procedure.
This diagnostic procedure combines an X-ray with an endoscope to look for diseases within the pancreas and bile ducts. The endoscope is inserted into the mouth or oesophagus and is used to visualize the pancreas and bile duct. The images produced by this procedure are then projected onto monitors.