How to Tell If You Have a Pancreatic Tumor?
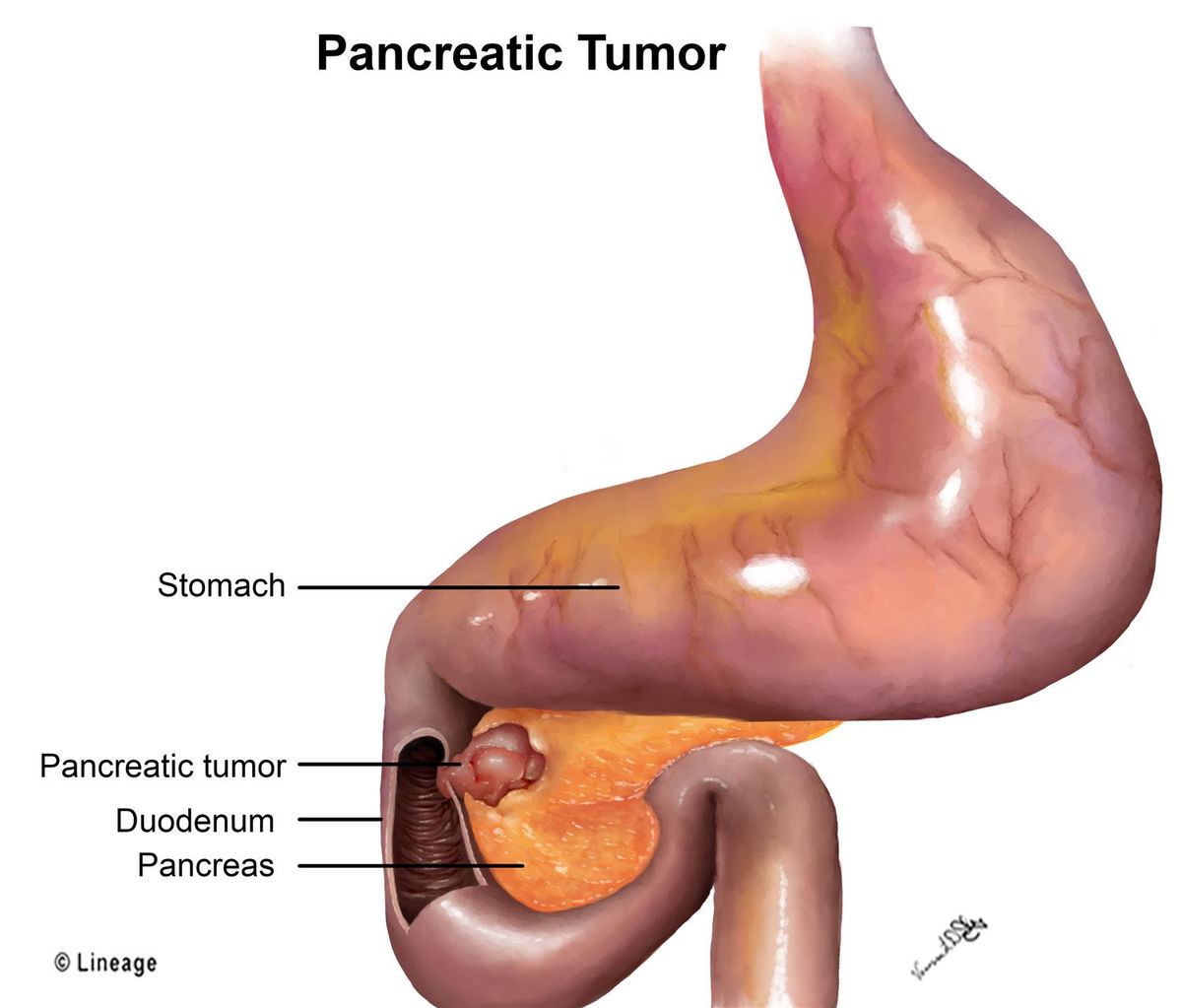
Endocrine and exocrine pancreatic tumors have distinct signs and symptoms. Both can be treated, and each type has its treatment options and prognosis. Endocrine tumors secrete insulin, while exocrine tumors produce hormones that help the body function properly. Here are some of the key differences between these types of pancreatic tumors. Read on to learn more. Also, learn to tell if you or a loved one has a pancreatic tumor.
Endocrine tumors
Endocrine tumors of the pancreas are less common than other types. They develop in the cells of the pancreas, known as neuroendocrine cells. Neuroendocrine cells are similar to nerve cells in some ways, but they also produce hormones. They are spread throughout the body. The symptoms of pancreatic cancer are often difficult to predict and may progress rapidly. However, diagnosing and treating these tumors without harming your overall health is possible.
Neuroendocrine tumors of the pancreas are most commonly treated with surgery. The surgical resection of these tumors is the most common treatment. In addition to surgery, chemotherapy and radiation are often used to reduce recurrence rates and control symptoms in metastatic tumors. Endocrine tumor treatments are performed by a multidisciplinary team comprised of endocrinologists, pancreatic neuroendocrine surgeons, radiologists, and nuclear medicine specialists.
Insulinomas
A biopsy is a diagnostic procedure wherein a healthcare provider takes cells and tissue samples from a patient's pancreas. Typically, this procedure is performed during an X-ray or ultrasound. In the case of insulinoma, a biopsy is required to determine whether the tumor is benign or malignant. There are three grades and stages of insulinoma. A low-grade tumor has cells that look normal, while a high-grade tumor has features in between. A grade three tumor has cells that look abnormal and multiply rapidly.
A diagnosis of insulinomas is crucial for any patient with a history of diabetes. If diagnosed early, insulinomas are rare and treatable. In most cases, a pancreatic tumor is cured with appropriate treatment. Despite the risk, a single insulinoma is a treatable condition. However, it is important to note that only 10% of insulinomas are malignant, which makes them a rare tumors to diagnose.
Squamous cell carcinoma
A 65-year-old Caucasian female presented with abdominal pain and obstructive jaundice. Her family history of pancreatic cancer was significant. Histopathology confirmed the diagnosis of SCC. CT scan revealed a 3.9-x-3.5-cm mass in the pancreatic head and enlarged peripancreatic lymph nodes. During EUS, a biliary stent was placed through the mass and the underlying peripancreatic duct. The biopsy revealed metastatic tumor cells arranged in nests. This disease was staged and performed.
Pancreatic squamous cell carcinoma has similar symptoms as adenocarcinoma. Patients with this disease often experience back pain, nausea, and anorexia. Other common symptoms include upper gastrointestinal bleeding and melena secondary to gastric invasion. Treatment options are unclear. While the primary site of SCC is the pancreas, this disease is generally thought to be metastatic from another organ.
Acinar cell carcinoma
This cancer is classified into atypical, squamous, and acinar cell types. Patients with ACC and PB have a similar appearance, but the differentiation lines of the tumor are different. One major difference between ACC and PB is the presence of squamoid nests in the tumor. Patients with ACC are more likely to have widespread metastatic disease and shorter overall survival.
Acinar cell carcinoma is found in all pancreas regions, including the liver. While it can occur anywhere, the patient presented with abdominal pain. Imaging is essential for determining whether the tumor is a single mass or if it has spread to other organs. Computerized tomography (CT) can help determine the primary lesion and its metastatic potential. Diagnosing ACC early is key for the patient's overall survival.