Conquering the Unknown: Unveiling the Mysteries of Primary Biliary Cholangitis
Discover Primary Biliary Cholangitis, a rare autoimmune liver disease affecting bile ducts, causing liver damage, cirrhosis, and various symptoms.
Primary biliary cholangitis (PBC) is a chronic and progressive liver disease that primarily affects middle-aged women. Although it is relatively rare, PBC can lead to severe complications and even liver failure if left untreated. This blog post will discuss the causes, symptoms, diagnosis, and treatments for primary biliary cholangitis to help raise awareness and provide valuable information for those affected by this disease.
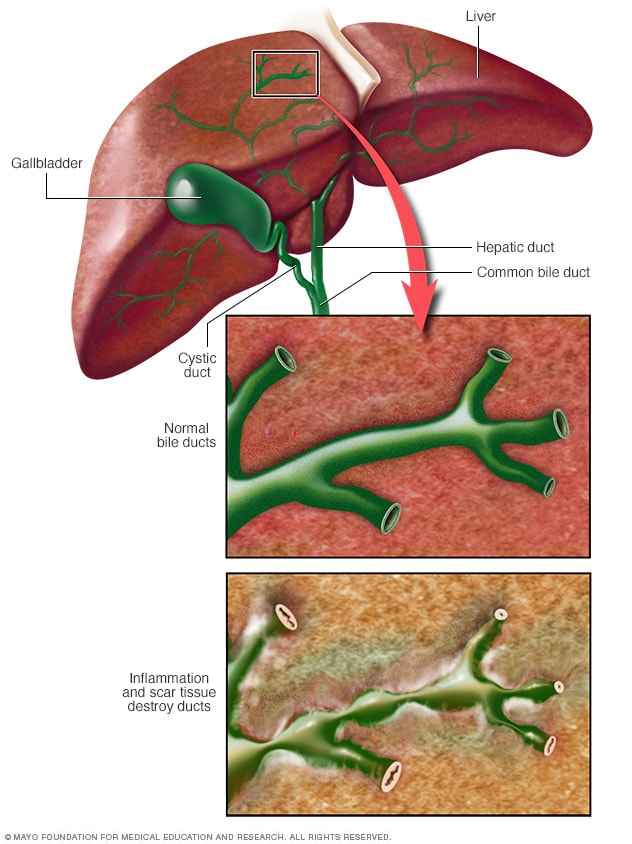
PBC is an autoimmune disease, which means that the body's immune system mistakenly attacks its own healthy tissues. In this case, the immune system specifically targets the bile ducts within the liver, causing inflammation and damage. Bile is a fluid produced by the liver that helps break down fats and eliminate waste products from the body. When bile ducts become damaged due to inflammation, bile can accumulate in the liver, leading to further injury and scarring, a condition known as cirrhosis. The exact cause of PBC remains unclear, although genetic factors and environmental triggers are believed to play a role in its development.
Early diagnosis of primary biliary cholangitis is crucial, as timely treatment can help slow down the progression of the disease and minimize complications. Symptoms of PBC can vary widely and often develop gradually, which can make it challenging to diagnose. Some common early symptoms include fatigue, itching (pruritus), and dry eyes or mouth. As the disease progresses, individuals may experience more severe symptoms such as jaundice (yellowing of the skin and eyes), fluid buildup in the abdomen, and mental confusion. If you are experiencing any of these symptoms, it is essential to consult with your healthcare provider as soon as possible.
To diagnose primary biliary cholangitis, healthcare providers will typically start by reviewing the patient's medical history and performing a physical examination. Blood tests are often ordered to assess liver function and check for the presence of specific autoantibodies associated with PBC. Imaging studies, such as an ultrasound or magnetic resonance imaging (MRI), may also be required to rule out other potential causes of liver problems. In some cases, a liver biopsy may be necessary to confirm the diagnosis and assess the extent of liver damage.
There is currently no cure for primary biliary cholangitis, but various treatments are available to help manage symptoms and slow down the progression of the disease. The mainstay of treatment for PBC is a medication called ursodeoxycholic acid (UDCA), which works by promoting the flow of bile and reducing inflammation in the liver. In some cases, UDCA may not be effective, and other medications, such as obeticholic acid, may be prescribed as an addition or alternative. It is essential to carefully monitor the liver function of individuals with PBC and adjust treatment plans accordingly.
In addition to medications, lifestyle changes and supportive therapies can also help manage PBC and improve overall quality of life. Maintaining a healthy diet, staying physically active, and getting enough rest are crucial for individuals affected by this disease. Additionally, specific treatments may be necessary to address complications that can arise from PBC, such as osteoporosis and vitamin deficiencies. In cases of advanced liver failure, a liver transplant may be the only option to improve survival and quality of life.
In conclusion, primary biliary cholangitis is a rare but serious liver disease that requires prompt diagnosis and treatment to prevent complications and preserve liver function. By raising awareness about PBC and encouraging individuals to seek medical care if they experience concerning symptoms, we can improve the prognosis for those affected by this challenging disease.