Cellular Immunity
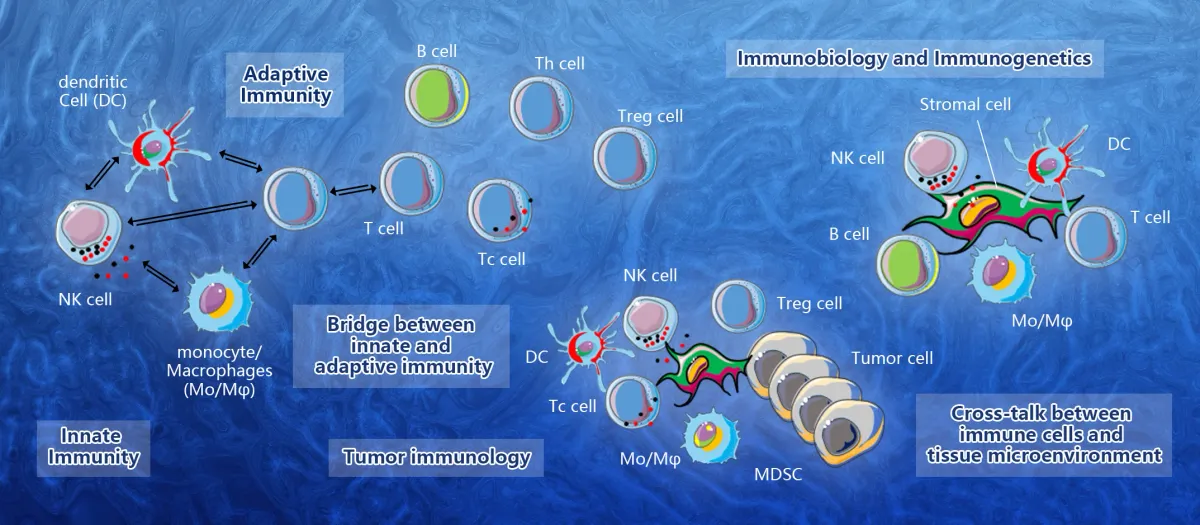
Cellular immunity involves a complex network of lymphocytes. These cells are made up of three types: naive T cells (T cells that do not produce antibodies), helper T cells (T cells that make antibodies), and killer T cells (T cells that produce antibodies). All three types have varying degrees of sensitivity and are regulated by certain proteins called cytokines. These proteins can damage the target cell directly or activate "killer" T cells.
Adaptation to high parasitism rates
Populations with high parasitism rates exhibit distinct cellular immune response patterns. For example, lamellocytes are more active in people with high parasitism than in those with low parasitism rates. These differences are attributed to the expression of two different antigens, alpha-PS4 and my. These antibodies recognize immature lamellocytes and mature lamellocytes, respectively.
Environmental conditions largely determine adaptation to high parasitism rates. Warmer temperatures favor parasite life-cycle completion, thereby increasing pressure on hosts. During a 2003 European heat wave, sticklebacks exposed to higher temperatures had higher parasite burdens, which reduced their growth rates and increased mortality. Compared with colder climates, sticklebacks exposed to 21 degC experienced higher parasite burdens.
Direct lysis of virus-infected cells
The direct lysis of virus-infected cells is one of the most important tools for cellular immunity. This process is selective against HIV infection and affects the development of HIV virions. In the early stages of the disease, CD8+ T cells can act against HIV particles. This process is triggered about 12 hours before the budding of new viral particles. Cells that express HIV Nef protein are particularly susceptible to lysis by CTLs. This susceptibility correlates with the expression of viral proteins in the cell and occurs before the extracellular virus production. Granzymes and perforin mediate this process. In addition, some CTLs also use the Fas ligand.
In ADCC, effector leukocytes recognize the Fc portion of IgG molecules on target cells. The effector cell then binds to this Fc protein and lyses the infected cell. This method is extremely efficient for direct lysis of virus-infected cells and requires far fewer antibodies than antibody-complement lysis.
Humoral immunity vs. cell-mediated immunity
Cellular and humoral immunity function differently, but both works to protect the body against infection and pathogens. The body fights against pathogens in cell-mediated immunity by producing antibodies and other substances that react to their antigens. Cellular immunity is mediated by T-cells and B-cells, which have different functions. Humoral immunity is a defense mechanism against bacteria and intracellular pathogens in body fluids, while cell-mediated immunity attacks pathogens inside the body.
Humoral immunity consists of the production of antibodies from B lymphocytes that mature into plasma cells. Cell-mediated immunity, on the other hand, involves T-cells and antibodies. B-lymphocytes are produced in the bone marrow, while T-lymphocytes mature in the thymus.
Mechanisms of antigen neutralization by effector T-cells
In cellular immunity, effector T-cells recognize and neutralize antigens. The process involves soluble factors, phagocytic cells, killer cells, and antibodies produced by B cells. It is the result of this inflammatory response that enables the immune system to create an immune memory.
These effector T-cells recognize antigens and bind them to the MHC molecules in the body. These cells are a part of the adaptive immune response, but they are much slower than the innate immune system. Therefore, they require information from the natural immune system and must develop in the presence of antigens. Once antigens are identified, they are displayed by APCs on the body's surface and stimulate B cells, which differentiate into plasma cells. After a while, these effector T-cells can induce apoptosis in intracellularly infected or cancerous cells. They can also be memory cells, which persist in circulation after the primary exposure to a pathogen.
Influence of immune modulators on cellular immunity
Immunomodulators alter the body's immune response. There are two types of immunomodulators: immunostimulants and immunosuppressants. The former enhances the immune response to a particular pathogen, while immunosuppressants inhibit the immune response. Examples of immunosuppressants include monoclonal antibodies used in cancer treatment and tyrosine kinase inhibitors used to treat leukemias and gastrointestinal tumors. Another type of immunomodulator is an interleukin, which mimics the effects of natural interferons and inhibits the immune response.
Immunosuppressants work by regulating cytokines and blocking viral replication. They also stimulate the production of cytokines, which support adaptive immunity. They are a class of drugs with multiple effector cells and mediators. The cytokines released by these cells inhibit the growth of bacteria and other pathogens.