Benefits and Limitations of EUS-FNA for Pancreatic Cancer
The procedure requires accurate positioning of the pancreas. As the pancreas moves with each breath, this positioning is essential for accurate results. In addition, intestinal cleansing is necessary before ultrasound therapy. Gas or constipation can interfere with positioning, causing ultrasound waves to scatter and damaging the adjacent intestines. Therefore, patients with gas should undergo an invasive bowel cleansing before ultrasound treatment.
Focused ultrasound hyperthermia
HIFU is a focused ultrasound therapy that involves heating a specific area using sound waves. HIFU is most effective when the heat source is placed within a defined region and does not damage collateral tissue. It is also a highly accurate form of treatment when MR guidance is used. In addition, several studies have shown that HIFU can deliver targeted drugs in solid tumors. This treatment combines TSL with HIFU and shows promising results in treating PDA.
In clinical trials, high-intensity focused ultrasound has increased mesenteric vessel patency in patients with advanced pancreatic cancer. Moreover, this therapy is effective when combined with chemotherapy. Researchers from the University of Tokyo have shown that focused ultrasound can significantly improve survival for patients with advanced pancreatic cancer. These patients will not require surgery or radiation because it is non-invasive.
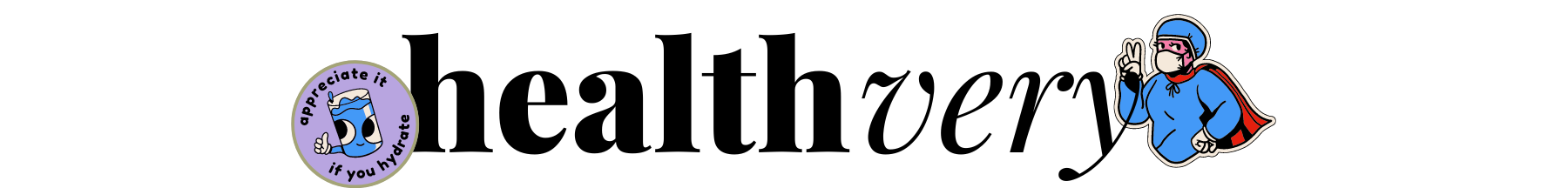
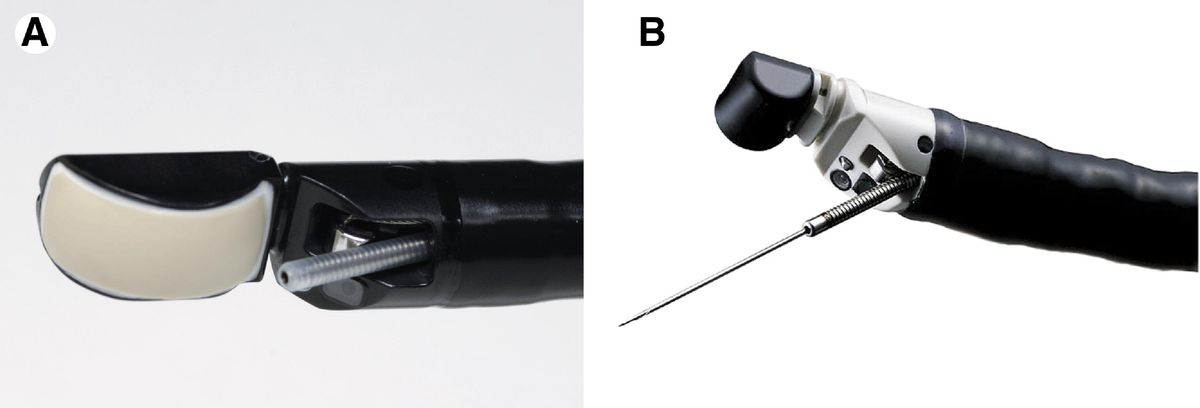
EUS-FNA
Endoscopic ultrasound has been widely adopted in many interventional procedures and strategies for diagnosing and staging gastrointestinal (GI) cancers. EUS-FNA for pancreatic cancer is considered a valuable tool to diagnose cancer and distinguish between benign and malignant cysts. Its use is highly recommended for pancreatic cancer patients with difficulty performing needle biopsies for various reasons. This article discusses the benefits and limitations of EUS-FNA in treating pancreatic cancer.
Although CT remains the gold standard for diagnosing chronic pancreatitis, EUS is a valuable adjunct for visualization of less progressive changes. EUS-FNA is also helpful for the diagnosis of focal lesions in the pancreas. The EUS image is analyzed by digital image analysis, reducing the role of the endoscopist. The color and pattern of individual pixels are taken into account by algorithms. Furthermore, EUS elastography determines the tissue's hardness when it responds to compression.
HIFU
To assess HIFU in pancreatic cancer, an ultrasound imaging specialist uses a specialized transducer to target the tumor. The US image is acquired in slices, with the probe moving through the pancreatic tumor. Blood pressure, pulse rate, and peripheral oxygen saturation were monitored during the procedure. One study demonstrated that the treatment was safe and effective for many patients with pancreatic cancer.
In clinical trials, HIFU treatment has shown promising results in patients with advanced-stage pancreatic cancer. The risks and complications associated with this treatment are low compared to minimally invasive thermal ablation approaches and radiation therapy. In general, complications such as abdominal pain, subcutaneous fat sclerosis, and rash were mild and resolved within a short time. However, a single study reported that three patients suffered severe complications after HIFU therapy, including portal vein thrombosis, pancreaticoduodenal fistula, and obstructive jaundice.